Friday, November 25, 2016
Podcast Hosting Page
This is where we are storing/hosting podcast links. Bear with us - content coming soon!
Sunday, February 7, 2016
Observing motor control and movement quality
Purpose:
Describe how GRIP Approach evaluates movement quality based on physics and motor control.
Think about the basic activity of transitioning from sitting position to standing. Clinicians, therapists, and trainers may have 2 main pathways of observing this movement critically.
Observation Path # 1
We get in trouble in a few areas.
I'd like to redefine pain as the personal experience in response to nociception or perceived danger. Essentially pain is entirely subjective for everyone and can be in response to real tissue damage and danger as reported to the brain by stimulation of nociceptors or in response to perceived danger such as a knee that is still painful to bend because it previously was inflamed stimulating nociceptors to send afferent information to the brain which was then interpreted as pain (even in an injury that is 20 years healed). Subjective pain is not an accurate way of judging movement quality. We'd like to shelve the subjective experience of pain to talk in terms of function and physics. For more on pain, Lorimor Moseley and Gregory Lehman have a few articles below:
https://theconversation.com/explainer-what-is-pain-and-what-is-happening-when-we-feel-it-49040
http://www.greglehman.ca/2015/01/04/smudging-pain-neurotags-and-cortical-body-maps-explaining-the-weirdness-of-pain/
The whole concept of movement quality also poses some concrete challenges, most notably, defining adequate or proper moment quality. These definitions tend to focus on specific positions, movements, and firing patterns based on averages that the observer deems to be ideal. It leaves me searching for the beautiful specificity of each person. Where does specific anatomy, training, and previous patient experience squeeze into the picture. Here is where GRIP comes in.

Choice of muscle - Does your brain think you need the monster truck or the unicycle?
When we look at the design elements of muscles a few things jump out:
Cross-sectional area of skeletal muscle is proportional to muscle strength. Sarcomeres generate contractile force - the greater the sarcomere count the greater force can be generated by the tissue.
The further away the the muscle is from your center of mass and the rotational reference point that it controls, the greater compression force is generated. If we use the lumbar spine for example, the iliocostalis can generate a greater force on the spine than the multifidus with same contractile effort due to the greater moment arm of the iliocostalis (perpendicular distance from the muscle to the point of rotation)


Thank you Aaron Swanson for the diagrams!
So if we look at the design of muscles, we see that big muscles near the surface of our body are both the strongest and the most capable of generating compressive force on our joints. These muscles are most capable of meeting huge increases in demand. GRIP's assumption is that your brain (specific, I know!) recruits more units and those units of greater cross-sectional area further from the rotational axis in response to perceived need/increased demand.

So if our bodies were infinitely durable or could be replaced easily, the most effective system of movement and postural control would be primarily these phasic muscles near the surface that are large. The two issues with this are that 1) these muscles tend to cross multiple joints making them less capable of skilled movements and that 2) the body is not insanely durable. Pavement holds up better to unicycles than monster trucks.
Describe how GRIP Approach evaluates movement quality based on physics and motor control.
Observation Path # 1
- Can the person transition from sitting to standing position without help?
- Can he/she do so with or without experiencing pain?
- Can he/she do so several times?
Observation Path # 2
- Does the person have proper movement quality during the transition from sitting to standing?
- What position are the joints in?
- What is the firing order of the musculature?
- Does the body have to work around a structural barrier to achieve the movement?
- Etc., Etc.,
- Can I increase demand to this transition without negatively altering movement quality?
Observation path # 1 is all most clients care about and is a fine observational path. Most current rehabilitation methodology focuses on observation path # 2, noting one cannot perform sitting to standing several times for a lifetime without appropriate movement quality. This is also a fine observational path as certain movements have been associated with a higher occurrence of injury.
We get in trouble in a few areas.
I'd like to redefine pain as the personal experience in response to nociception or perceived danger. Essentially pain is entirely subjective for everyone and can be in response to real tissue damage and danger as reported to the brain by stimulation of nociceptors or in response to perceived danger such as a knee that is still painful to bend because it previously was inflamed stimulating nociceptors to send afferent information to the brain which was then interpreted as pain (even in an injury that is 20 years healed). Subjective pain is not an accurate way of judging movement quality. We'd like to shelve the subjective experience of pain to talk in terms of function and physics. For more on pain, Lorimor Moseley and Gregory Lehman have a few articles below:
https://theconversation.com/explainer-what-is-pain-and-what-is-happening-when-we-feel-it-49040
http://www.greglehman.ca/2015/01/04/smudging-pain-neurotags-and-cortical-body-maps-explaining-the-weirdness-of-pain/
The whole concept of movement quality also poses some concrete challenges, most notably, defining adequate or proper moment quality. These definitions tend to focus on specific positions, movements, and firing patterns based on averages that the observer deems to be ideal. It leaves me searching for the beautiful specificity of each person. Where does specific anatomy, training, and previous patient experience squeeze into the picture. Here is where GRIP comes in.

Theory: 'Optimal' motor control can be observed in individuals based on evaluation of the balanced recruitment of musculature surrounding a joint or region in question. This is specific to the individual but follows predictable patterns outlined in developmental kinesiology and respects anatomical variations.
Choice of muscle - Does your brain think you need the monster truck or the unicycle?
Phasic musculature?
Postural musculature?
Cross-sectional area of skeletal muscle is proportional to muscle strength. Sarcomeres generate contractile force - the greater the sarcomere count the greater force can be generated by the tissue.
The further away the the muscle is from your center of mass and the rotational reference point that it controls, the greater compression force is generated. If we use the lumbar spine for example, the iliocostalis can generate a greater force on the spine than the multifidus with same contractile effort due to the greater moment arm of the iliocostalis (perpendicular distance from the muscle to the point of rotation)


Thank you Aaron Swanson for the diagrams!
So if we look at the design of muscles, we see that big muscles near the surface of our body are both the strongest and the most capable of generating compressive force on our joints. These muscles are most capable of meeting huge increases in demand. GRIP's assumption is that your brain (specific, I know!) recruits more units and those units of greater cross-sectional area further from the rotational axis in response to perceived need/increased demand.

So if our bodies were infinitely durable or could be replaced easily, the most effective system of movement and postural control would be primarily these phasic muscles near the surface that are large. The two issues with this are that 1) these muscles tend to cross multiple joints making them less capable of skilled movements and that 2) the body is not insanely durable. Pavement holds up better to unicycles than monster trucks.
If activities like sitting, standing, and walking can be performed with adequate motor recruitment (rather than excessive) we greatly reduce the compressive and shearing forces at the joint. When a demanding activity requires extensive motor recruitment, we expect synergy and balance to provide a centrated position, essentially centering the compressive force for the benefit of a neutral force dispersement.
If there is excessive motor recruitment and a clenching/compression strategy in the basic activities of sitting, standing, and walking it becomes infinitely more difficult to produce an adequate response of synergy and balance when demand increases. I always say in my courses, “your program of control, wether clenching or expanding, is going to increase and spread throughout the body when you increase demand”. We see this in every day examples. Stand up and actively squeeze the toes of your feet together to grip the ground. Take a few steps. Notice how this creates a small clenching response at the knee, hamstrings, and throughout the rest of the kinematic chain. Now spread and elongate your toes and notice how the motor recruitment changes. The clenching dissipates. The breath relaxes. This is an example of how the motor control of stabilization spreads throughout the body with increased demand. Now, in this simple example of walking with a concentric/superficial strategy of stabilization vs an elongation/expansion strategy, we observe and hypothesize a difference in shearing and compressive forces at the joint.
So, am I saying we need to turn in our monster trucks for unicycles? No, absolutely not! These surface muscles are our prime movers and are positioned well for power. We need to use them, train them, strengthen them, but to be cognizant of their ability to generate insanely high compressive and shearing forces on the joints of the body. These tissues need to be recruited appropriately and balanced around the joint to disperse the force transmitted. This is where we see the curve of a spinal segment being less clinically significant to an injured disc in question than strategy of stabilization around that joint.
Bringing it all home here: When there is a perceived increase in demand (poor joint position, posture, increased external load, etc.) we recruit the big surface muscles to meet the demand. When there is less perceived demand we recruit less superficial musculature. When over-recruitment of these phasic muscles are used as a primary stabilization strategy we generate adverse compressive and shearing forces. This is poor motor control and can be seen in those with brain injuries, cerebral palsy, central developmental disturbances, and at varying degrees with all of our patients.
So how can we apply this observation to our clinical model on a daily basis? Evaluate the individual in their necessary movements of life and in your favorite screens for the balance of musculature around a joint in question, the appropriate level motor recruitment recruitment, absence/presence of a clenching/compression stabilization strategy, and their ability to maintain this balance with increased external load.
To explore these concepts with practical clinical and performance applications sign up for a course at www.GRIPapproach.com
So, am I saying we need to turn in our monster trucks for unicycles? No, absolutely not! These surface muscles are our prime movers and are positioned well for power. We need to use them, train them, strengthen them, but to be cognizant of their ability to generate insanely high compressive and shearing forces on the joints of the body. These tissues need to be recruited appropriately and balanced around the joint to disperse the force transmitted. This is where we see the curve of a spinal segment being less clinically significant to an injured disc in question than strategy of stabilization around that joint.
Bringing it all home here: When there is a perceived increase in demand (poor joint position, posture, increased external load, etc.) we recruit the big surface muscles to meet the demand. When there is less perceived demand we recruit less superficial musculature. When over-recruitment of these phasic muscles are used as a primary stabilization strategy we generate adverse compressive and shearing forces. This is poor motor control and can be seen in those with brain injuries, cerebral palsy, central developmental disturbances, and at varying degrees with all of our patients.
So how can we apply this observation to our clinical model on a daily basis? Evaluate the individual in their necessary movements of life and in your favorite screens for the balance of musculature around a joint in question, the appropriate level motor recruitment recruitment, absence/presence of a clenching/compression stabilization strategy, and their ability to maintain this balance with increased external load.
To explore these concepts with practical clinical and performance applications sign up for a course at www.GRIPapproach.com
Monday, April 22, 2013
The Fascinating & Frustrating FASCIA
Fascia is one of those buzzwords right now. We had to jump aboard! But is fascia just another fascinating and frustrating fad in manual medicine?
10 years ago, it would have been tough to name a handful of manual therapists in a given area that utilized Mckenzie Diagnosis and Therapy, Dynamic Neuromuscular Stabilization (DNS), Functional Screening (FMS, SFMA, Janda's Screens, etc.), Active Release Techniques, or even performance based rehabilitation of common MSK problems. It is now hard to find a handful that don't apply at least one or two of these (thankfully!). This is partially due to how rapidly information travels now due to social media and websites and partially due to the wonderful research backing a functional -active model of care.
We are now at the forefront of another area of research that will shape manual medicine for the next decade and beyond. What a thrilling time to be in this form of healthcare! In 2007, the first International Fascial Research Conference was held at Harvard Medical School. The emphasis and centerpiece of this conference was the presentation of the latest and best scientific fascia research for clinical professionals in whose specialties the human fascia are central in both theory and practice. Many of the scientists attending had little experience with clinical practice and clinicians were often unfamiliar with each other's work. (1) This proved to be groundbreaking exposure for the 650 persons in attendance. This sparked a movement for researchers and clinicians alike! The International Fascia Research Congress was held again in 2009 and 2012 with rapidly improving study designs and presentations. The congress is now accompanied by practical workshops and training, which accelerates the movement of findings from the lab into the clinic.
In many ways, the research has highlighted what we have always known: "(tune) The hip bone is connected to the back bone..."- muscles are connected together via fascia to form slings for movement - when fascia is aggravated it becomes less pliable and generates pain - treating the fascia can normalize the surrounding structures - etc. etc. etc. But in many exciting ways this research was entirely new. For example; new research shed light on the connection of fascia not only within a group of muscles that fire together, but from the 3rd toe of the right foot all the way through the body to the third finger of the opposite arm (Wow, cool!). Furthermore, this fascia could be traced from just under the skin through several layers of tissues, across axes of movement, and actually into the viscera and organs!!! There finally seemed to be scientific proof and reasoning behind the many theories of muscle-to-organ connections. Could a faulty movement pattern truly and reliably start a cascade of visceral dysfunction via fascial connections? Can the newly defined fascial connections to the intervertebral disc be treated to relieve discogenic pain and centrate the joint? I'll let you peruse the research. What was most groundbreaking to me, was the consistency and reliability of the findings presented - especially those focusing on myofascial pain and dysfunction. Numerous symptoms that appear randomly scattered throughout a patient's body and psyche now had a tactile, visual, well-researched connection. Groundbreaking. Earth shattering.
These findings and many others from the congress leave the hardworking, dedicated, and curious therapist with a major question: "How can I apply this research in my clinical practice to help patients with the trickiest pain and dysfunction"? Well, I am glad you asked! This is what the 2014 Course Calendar for GRIP Approach is all about. Getting the best researched and best taught approaches into your hands and seeing the difference in your patients and your practice!
We will announce our full 2014 Course Calendar in a few weeks. With over 8 fascia driven courses already confirmed, this is sure to be another great year! You won't find any single-muscle, single-joint, or single-symptom treatments in these courses. Our courses will teach you to reliably break down the most complicated global issues and cure (not manage) their underlying cause with minimal visits. These courses are designed to give you an answer to your hardest clinical questions and dramatically improve your results in patient care. Stay tuned for updates! www.gripapproach.com
1) First International Fascial Research Conference, http://www.fasciacongress.org/2007/
Exciting Links for Fascia
http://www.fasciacongress.org/
http://www.fascialmanipulation.com/
http://www.leonchaitow.com/fascia.htm
Friday, December 28, 2012
The Janda Approach
GRIP Approach is pleased to present ‘The Janda Approach To Musculoskeletal Pain Syndromes’ as taught by his long time pupil Robert Lardner, PT
“Protective reflexes serve as the basis for all human movement and dominate in Pathology” – Janda
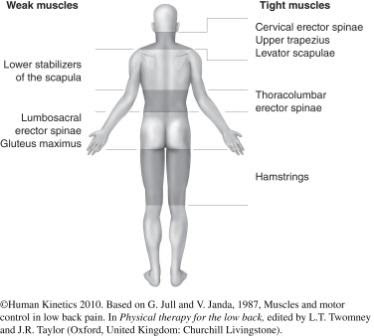
 Vladimir Janda Md, DSC is considered to be the father of
Czech rehabilitation and one of a handful of physicians responsible for how the
rehabilitation field was shaped internationally. He systematically defined
characteristic and predictable muscle imbalance syndromes in relationship to
the adaptations of the CNS and the ensuing chronicity – something we commonly
call ‘Janda’s crossed syndromes’. He viewed the sensory motor system as an
indivisible unit and stressed that effective treatment and the rehabilitation process
would have to respect this unity and its implications. His teachings influenced
many people, including Robert Lardner who co-authored the book ‘Assessment and
Treatment of Muscle Imbalance – The Janda Approach’.
Vladimir Janda Md, DSC is considered to be the father of
Czech rehabilitation and one of a handful of physicians responsible for how the
rehabilitation field was shaped internationally. He systematically defined
characteristic and predictable muscle imbalance syndromes in relationship to
the adaptations of the CNS and the ensuing chronicity – something we commonly
call ‘Janda’s crossed syndromes’. He viewed the sensory motor system as an
indivisible unit and stressed that effective treatment and the rehabilitation process
would have to respect this unity and its implications. His teachings influenced
many people, including Robert Lardner who co-authored the book ‘Assessment and
Treatment of Muscle Imbalance – The Janda Approach’.
This unique 2-day lab intensive will introduce the main
theories, concepts, and research of Dr Janda. Significant time will then be
spent in hands-on lab learning diagnosis according to Janda via visual
inspection, gait analysis, movement patterns, muscle quality, and trigger
points. The final half of the seminar will be spent learning Janda’s treatment
methods, normalization techniques, activation techniques, and sensorimotor
training. This intensive promises to greatly enhance your understanding and
abilities of treating musculoskeletal pain syndromes, and offer many additional
clinical pearls from Robert Lardner.
For details and registration visit our website.
For more information about Dr Janda, visit the website of
his US students and read this tribute paper.
Robert Lardner was born in Nigeria in 1961. His first career
was as a professional ballet and modern dancer after studying at the Rambert
Ballet Academy outside London, England. Going back to University he graduated
from the Department of Physical Therapy, Lund’s University, Sweden in 1991. He
has worked in several in- and out- patient rehabilitation facilities in Sweden
prior to moving to the United States in 1992.
Having been a staff physical therapist at McNeal Hospital,
Clearing Industrial Clinic, and a physical Therapy supervisor at Mercy
Hospital, He has also been in charge of physical therapy services at a number
of private outpatient and sports clinics.
He has studied extensively with Professors
Janda, Lewit and Kolar from the Czech Republic who are pioneers of functional
rehabilitation and manual medicine and who have strongly influenced his
philosophy and practice of physical therapy. He is a member of the
International College of Applied Kinesiology (ICAK). Currently, he is in
private practice in Chicago and teaches various rehabilitation seminars
throughout the United States and Europe.Monday, December 3, 2012
Dr Pavel Kolar presents his Dynamic Neuromuscular Stabilization (DNS) in a 4–course Chicago Summit!
We are pleased to announce that Dr Kolar and his faculty
will be presenting DNS A, B, C and Sport Course 1 in Chicago in October 2013.
The principles of DNS lay the groundwork to understanding habilitation, which
leads to excelling at rehabilitation. The attendee will leave with a unique
skill set, to diagnose and treat patients with deviations from ideal
development. These deviations from ideal present in our everyday patients - in
adults, children, athletes, and those with neurological injuries. This is an
important opportunity to learn an approach that not only stands on its own, but
also strengthens the diagnosis and treatment methods we currently employ.
Read more at www.gripapproach.com
Subscribe to:
Posts (Atom)